Reflecting on an Epidemic...40 Years Later
As the world is gripped by the coronavirus pandemic, 2021 marks the anniversary of our first encounter with another dreaded global disease. It’s been 40 years since HIV/AIDS was first identified in the United States.
“HIV may not have been as easily transmissible as infections like coronavirus or influenza, but in the 1980s, the reality was that if you did contract HIV, it was 100 percent fatal,” said Dennis Metzger, PhD, professor and director of the Department of Immunology and Microbial Disease.
HIV, a virus that attacks the immune system, wasn’t airborne or living on surfaces in the grocery store or on door knobs, instead it was transmitted through body fluids such as blood, rendering unprotected sex, blood transfusions and sharing needles a risk. Dr. Metzger said like coronavirus, asymptomatic people could transmit the virus, but, unlike coronavirus, HIV had a years-long asymptomatic incubation period in which people could unknowingly infect others.
AIDS first came into the public eye in 1981 when gay men began dying of a mysterious illness. By 1985, AIDS revealed itself to be deadly to all segments of the population.
“1981 is when we first recognized it in the United States, but HIV was probably in humans for much longer,” said Dr. Metzger.
Vincent P. Verdile, MD, dean of Albany Medical College and senior executive vice president, graduated from Albany Medical College in 1984.
“When I started med school, we did not even know what HIV/AIDS was. We only knew that young men were wasting away and dying in large numbers around the world. By the time I graduated, the disease had a name, but there was no treatment and no cure. It is hard to describe how frightening and frustrating this was for physicians, especially emergency physicians like me. We worried for our patients and our colleagues. We became more mindful of things like contact with blood, of the importance of personal protective equipment, of screening blood donors.”
“It is not an understatement to say that AIDS changed how we practiced medicine,” Dr. Verdile said.
Those mitigation methods we hear so much about in the age of Covid, including the use of PPE, testing and contact tracing, were all accelerated in the 1980s in response to HIV.
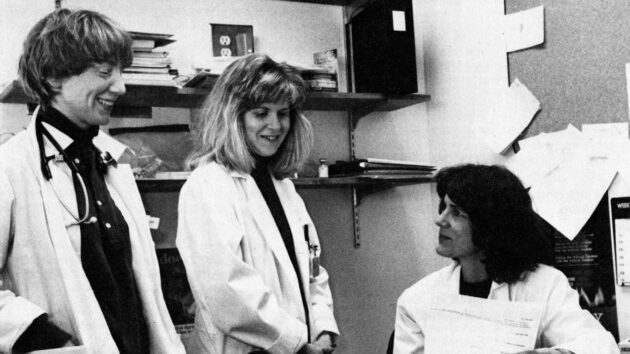
Because Albany Med began treating AIDS patients in 1981, the HIV Medicine program became, and remains, a national leader, having been involved with significant advances in medication and treatment. In 1987, Albany Med became one of the first state-designated treatment facilities, the first in upstate New York, and two years later began to focus more heavily on drug and clinical research, which helped lead to the development of ddC (HIVID) and ddI (Videx), two early medications. By 1996, introduction of the “drug cocktail,” a combination of 18 to 20 virus-fighting pills, caused a significant drop in mortality.
“It was miraculous. There were patients who were wasting away and dying who are alive today. I will always be grateful to the scientists who worked hard to make that breakthrough happen,” said Cyndi Miller, MD, medical director of HIV Medicine, who joined the program in 1991 and has been instrumental in developing hospital policy and implementation for HIV testing and prophylaxis.
That early drug cocktail was followed by improvements in antiretroviral therapy that eventually led to fewer pills per day. Dr. Miller said while there is still no cure for HIV, with proper medical care, patients can live a normal lifespan.
“Today, 93 percent of our HIV patients have undetectable viral loads. That also means they cannot transmit HIV,” she said.
In 2014, PrEP (pre-exposure prophylaxis) drugs became available to effectively prevent at-risk people from contracting HIV.
Dr. Miller said that while treatment has advanced, stigma remains.
“People feel ashamed about contracting HIV. Sadly, we’re still fighting that part of it 40 years later,” she said.
Since 1990, Albany Med has been a recipient of funding from The Ryan White CARE Act, the largest federally funded program for people living with HIV/AIDS, meaning Albany Med can offer a comprehensive system of support services such as counseling and education, HIV primary medical care and medications for underserved patients.
Each year the Division of HIV Medicine sees about 1,500 patients from New York, Vermont and Massachusetts at its Albany and Kingston offices, a number that has remained steady. While several local facilities treat HIV/AIDS patients, Albany Med remains the only state-designated AIDS Center in the region.
Although advances in treatment and prevention have been stunning, doctors and scientists agree that development of an HIV vaccine is still the gold standard.
“Development of an effective HIV vaccine is a major priority but has been extremely difficult because the virus mutates very quickly, and it resides inside cells where vaccine-induced antibodies cannot reach it,” Dr. Metzger said. “However, clinical trials focused on HIV/AIDS vaccination continue around the world, and it is possible we will see some form of vaccine in the next several years.”